When my daughter was young, she washed her hands a lot. We might have poked what we thought was gentle fun at her, saying she was “a little bit OCD”. Later, she began to disclose “bad thoughts”, which I assumed were the typical products of a child’s imagination. I told her we all had thoughts like that, and if we ignored them, they went away.
Hers didn’t. At 21, they were out of control and out of proportion to anything like reality. She was diagnosed with obsessive-compulsive disorder and I finally realised there was nothing “a little bit” about this condition.
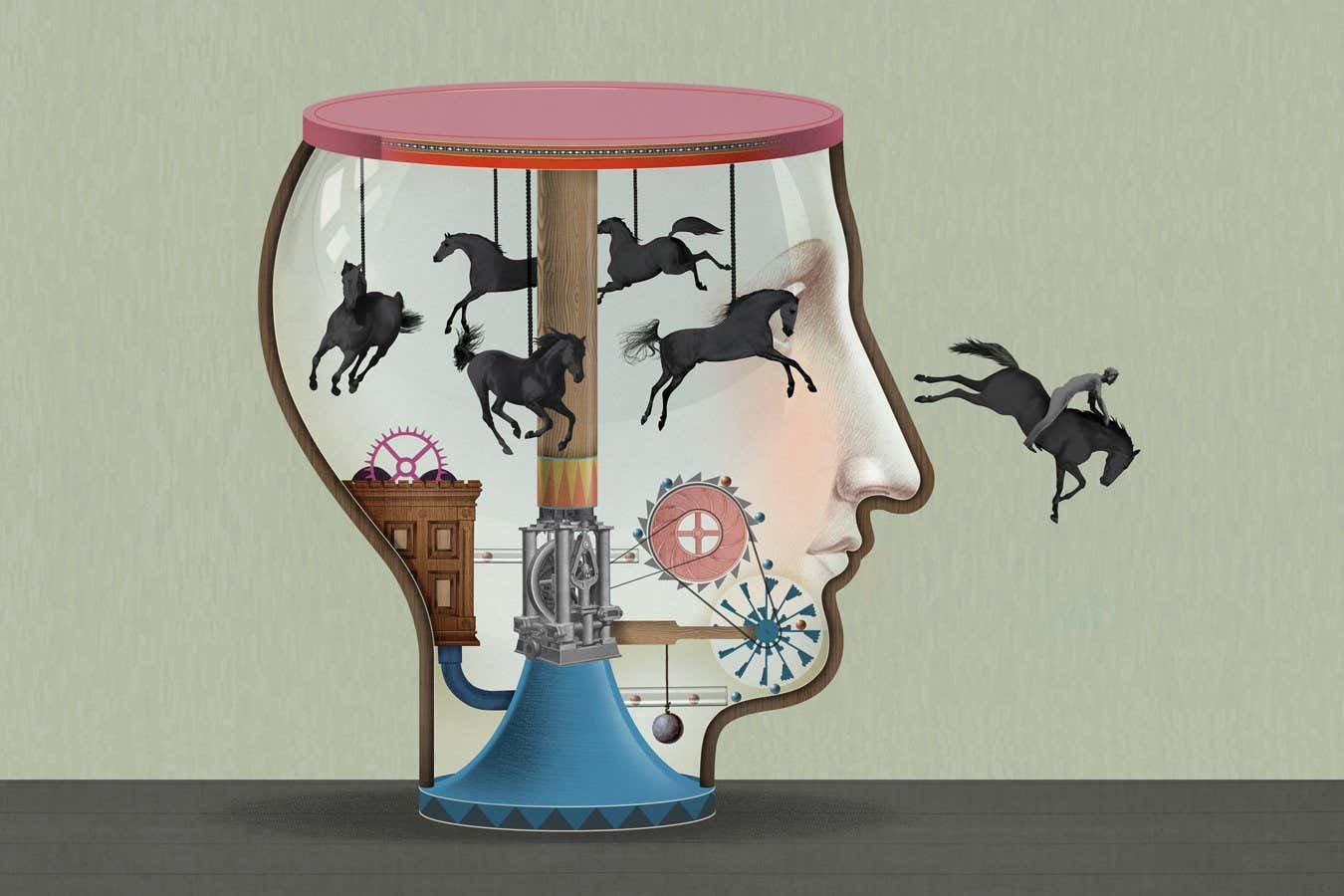
OCD is complex and commonly misunderstood, with a limited number of treatment options. But in recent years, the mechanisms in the brain and body that drive it are finally being pinned down, revealing an elaborate picture involving genetics, various brain networks, the immune system and even the bacteria in our gut. In turn, this growing understanding is opening up new possibilities of tackling this life-sabotaging condition.
Around the world, between 1 and 3 per cent of people are estimated to have OCD, which typically begins during adolescence or early adulthood. As its name suggests, it is characterised by obsessions – or intrusive thoughts – and compulsions, which are habits you can’t stop. “Compulsive thoughts capture attention and take over because they’ve become a compulsive habit,” says Barbara Sahakian at the University of Cambridge.…