More than 30,000 people in the United States alone have already received personalized CART-T-cell therapy for cancer.Credit: Qilai Shen/Bloomberg/Getty
When researchers first began to test engineered immune cells designed to fight cancer about 20 years ago, there was a scepticism. The scientific potential might be clear, but what about the economics of such a complex and specialized therapy? Each dose would have to be made afresh, with cells from an individual being shipped to a centralized laboratory, genetically engineered using sophisticated techniques and shipped back for reinfusion. The process would take too long and be too expensive. Regulators would also surely struggle to ensure the safety of such an involved, individualized process.
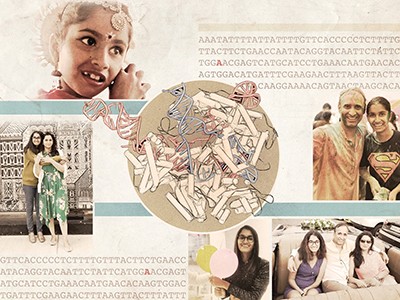
Today, the chatter is very different. Engineered CAR T immune cells have so far been used to treat more than 30,000 people with cancer in the United States alone. CAR-T therapy is being tested for other conditions, including some severe autoimmune disorders. As for commercial success, in 2023, CAR T cells earned biotechnology companies US$8.4 billion worldwide.
Two News Features in this issue describe other complex, bespoke therapies that, a decade ago, would have been considered infeasible, if not impossible. One is an mRNA cancer vaccine tailored to an individual’s tumour genome. The other is a CRISPR-based genome-editing therapy designed — but sadly never used — for one young woman with a rare neurological disorder.
How personalized cancer vaccines could keep tumours from coming back
Both approaches are fraught with challenges. As in the early days of CAR-T therapy, many of them are not scientific. But by guiding regulators and developing flexible platforms for producing bespoke treatments, researchers can help to shepherd therapies to the people who need them.
Researchers have long chased after vaccines that could rally the immune system against tumours, similarly to how vaccines rouse defences against pathogens. Companies can now sequence portions of a person’s tumour and select those most likely to be visible to the immune system. The mRNA molecules corresponding to those regions are synthesized, then encapsulated in fatty particles and injected — much like mRNA COVID-19 vaccines. From start to finish, the process takes as little as a month.
The technology behind these cancer vaccines is clinically more advanced than the genome editing used for some more specialized applications, for which researchers do not have the luxury of running large clinical trials. In one instance, scientists knew of only one person with the mutation they aimed to treat, using a technique called base editing that can make changes to specific DNA bases. It was, in effect, a treatment designed for a market of one person.
This kind of approach is called an n-of-1 therapy, a term that highlights the statistical challenges of interpreting results from a sample of one — not to mention the commercial challenge of designing and selling a therapy with a one-person market. But the name is potentially misleading and stigmatizing. A cancer vaccine based on an individual’s tumour could also be considered an n-of-1 therapy, yet this approach has attracted heavy investment from the pharmaceutical industry because the same process can be extended to many other people with cancer.
Hope, despair and CRISPR — the race to save one woman’s life
The same thinking is needed for genome-editing therapies for rare disorders. Some genetic conditions that weaken or disable the immune system could be grouped together, and therapies for these diseases designed and administered in the same manner, even if the specific DNA changes made are different. Identical or similar measures — such as levels of immune-cell function — could be used to determine how well the treatment works.
But for-profit companies cannot be relied on to develop such platforms for CRISPR-based therapies as long as the perceived market remains small. Some academic researchers are focusing on developing such platforms for CRISPR-based therapies. More should join them — or the chance to use genome editing to correct genetic disorders, the most severe of which are often rare, will be squandered.
Researchers can help regulatory agencies grappling with the new technologies. Regulators in the United States, the European Union, India and the United Kingdom have signalled a wish to aid the development of treatments for ultra-rare disorders. But they need help. Many regulations governing the manufacturing of therapies are grounded in regulatory paths forged years ago. Scientists can advise regulators on which technological advances have rendered certain cumbersome regulations unnecessary. This could speed up the development of treatments, as well as lower their costs.
Researchers around the world can engage in the same discussions with their regulators, and not just in typical hotspots for drug development, such as the United States and Europe. Such conversations will help to prepare for a future in which bespoke genetic therapies can be produced worldwide. They could also help to harmonize regulations between countries: an important goal for promoting the development of drugs for conditions that affect only a few individuals scattered around the globe.
As data accumulate from the treatment of people with rare genetic disorders, lessons learnt about the safety, effectiveness and manufacturing of bespoke therapies can be translated to treatments for more-common conditions. So the treatment of ultra-rare genetic disorders should not be devalued. Although a single disorder might affect only a few people, in aggregate, ultra-rare diseases affect millions. When it comes to personalized medicine, serving the interests of the few is in the interests of the many.